SOURCE: Social media users, Facebook, TikTok, 29 Sep. 2022
OTHER
REVIEW
On 29 September 2022, a Facebook user shared a TikTok video claiming that “Alzheimer’s most of the time is preventable. It’s not genetic, and it’s type 3 diabetes, which is insulin resistance of the brain”. The video claimed that “you become insulin-resistant in your whole body and then your brain becomes insulin-resistant” which makes “memories start to decline”. The clip received more than 13,000 interactions on Facebook and was shared 8,000 times.
The video implied that diabetes-related insulin resistance can cause Alzheimer’s disease. As we will explain in this review, this is unsupported by available scientific evidence. High levels of insulin and glucose in blood are associated with a higher risk of developing Alzheimer’s. However, the specific contribution of insulin dysregulation to brain damage in Alzheimer’s patients is still unclear. The video also contains some inaccuracies that we will show below.
Alzheimer’s disease is the most common neurodegenerative disorder worldwide. It is also the main cause of dementia, a group of symptoms that involve the loss of cognitive functioning—thinking, remembering, and reasoning—up to a point that interferes with the person’s daily life.
The World Health Organization estimates that dementia affects 55 million people worldwide, with ten million new cases per year. According to a 2022 annual report by the U.S. Alzheimer’s Association, more than 6.5 million people are living with Alzheimer’s in the U.S. However, the number of Alzheimer’s cases are projected to reach 12.7 million in the U.S. and more than 115 million worldwide by 2050, as the world’s number of people aged 60 and older, who are at a higher risk of Alzheimer’s, is expected to double by that time.
Alzheimer’s disease occurs when neurons within specific brain regions stop working correctly, lose connections with other neurons, and ultimately die. This damage seems to first affect the hippocampus and entorhinal cortex (see Figure 1), two connected brain areas involved in forming and retrieving memories. That might explain why the first symptoms of Alzheimer’s disease are usually a loss of memory and ability to perform certain tasks.
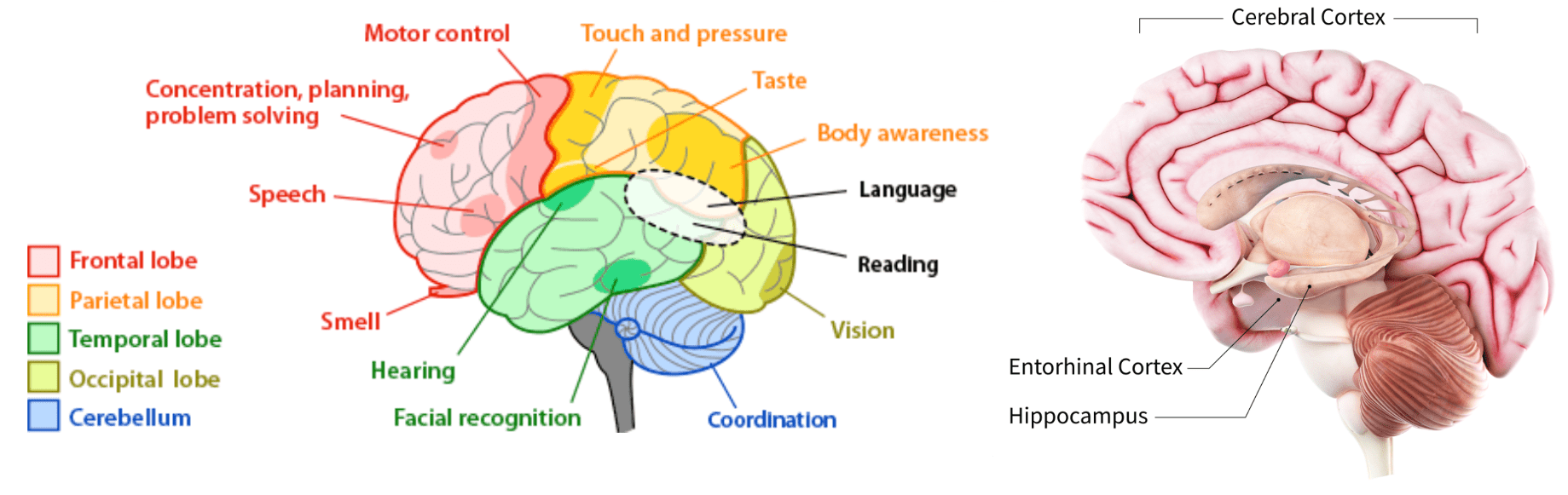
Figure 1. Left, parts of the human brain and specific functions they control. Source: Arizona State University. Right, brain regions most affected in Alzheimer’s disease. Source: U.S. National Institute of Aging.
Most patients start showing symptoms over the age of 65, which is known as late-onset Alzheimer’s disease. But around 10% of them present early-onset Alzheimer’s disease and develop symptoms between their 30s and 60s. However, multiple studies indicate that the molecular changes in the brain associated with the disease may start years or decades before the first symptoms appear[1,2].
One of these changes is the abnormal accumulation in the brain of two proteins called Tau and amyloid-beta. Fragments of amyloid-beta accumulate outside the neurons forming clumps called plaques. Inside the neurons, abnormal forms of Tau accumulate in structures called neurofibrillary tangles (see Figure 2). Plaques and tangles are hallmarks of Alzheimer’s, but it’s still unknown whether they are a cause of Alzheimer’s or a result of it.
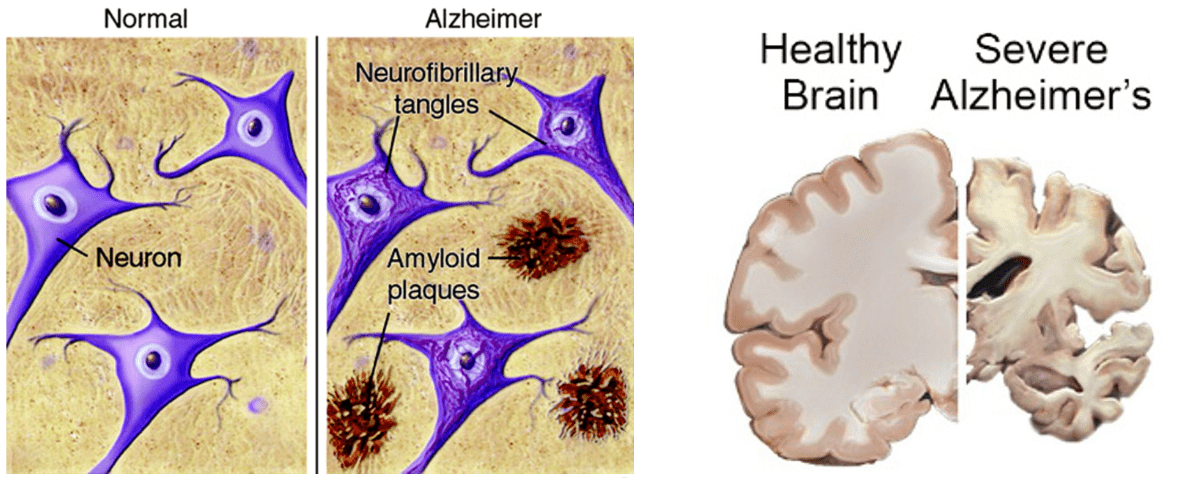
Figure 2. Left, representation of amyloid-beta plaques and neurofibrillary tangles in the brain of a healthy person and a person with Alzheimer’s disease[3]. Right, widespread brain damage and shrinking in the brain of a deceased Alzheimer’s patient. Source: U.S. National Institute of Aging.
As the disease progresses, neuronal damage spreads to regions of the brain cortex responsible for language, reasoning, and social behavior and ultimately to other brain areas, which begin to shrink (Figure 2). At late stages, patients have problems carrying out the most basic daily activities and are eventually completely incapacitated and dependent on others.
Contrary to what the video claimed, some cases of Alzheimer’s disease are genetic. Such cases account for 1% of the patients and are caused by specific mutations—changes in the genetic sequence—in three genes that provide the blueprint for the amyloid protein precursor (APP), or for presenilin 1 (PSEN1) and presenilin 2 (PSEN2), two proteins responsible for breaking down APP. These mutations result in the accumulation of amyloid-beta in the brain. People who inherit one of them will most probably develop early-onset Alzheimer’s disease.
Scientists don’t yet fully understand what causes late-onset Alzheimer’s. However, such cases are thought to result from a combination of multiple factors, including environmental, lifestyle, and genetic factors. Each of these factors influences the person’s likelihood of developing Alzheimer’s by either increasing the risk (risk factors) or reducing it (protective factors). Protective factors include genetics and lifestyle choices such as physical activity, cognitive stimulation, and a healthy diet.
Among the risk factors for Alzheimer’s, older age and genetics are the most important ones[4]. People who have one or more first-degree relatives with Alzheimer’s are more likely to develop the disease than those who don’t[5,6]. In fact, a study of more than 10,000 twin pairs indicated that genetic factors may account for as much as 80% of the risk of Alzheimer’s[7].
The most important genetic risk factor for Alzheimer’s involves the apolipoprotein E (APOE) gene, which provides the instructions to produce a protein that transports cholesterol and other fats in the bloodstream. There are three variants of APOE, but more than half of the people with Alzheimer’s carry the variant e4. This variant increases the risk of developing Alzheimer’s by about three to more than ten times, depending on whether the person inherits one or two copies of this variant—from one of the parents or from both of them[8]. Interestingly, the least common of the three variants (e2) has a protective effect.
In short, the claim that Alzheimer’s disease isn’t genetic is inaccurate because some early-onset cases are caused by mutations in one of three genes. This claim is also misleading because it disregards that the rest of the Alzheimer’s cases also have a strong genetic component, which sums to the effect of other contributing factors.
Diabetes is a chronic condition that causes glucose to accumulate at high levels in the blood. Glucose is the main source of energy that the cells use to carry out the biochemical reactions that keep us alive and healthy. The small intestine can directly absorb glucose from food into the bloodstream, at which point cells can take up glucose with the help of a hormone produced by the pancreas, called insulin.
People with diabetes can’t process glucose properly, either because the person doesn’t produce insulin (type 1 diabetes) or because the cells don’t respond well to it (type 2 diabetes). The latter case is known as peripheral insulin resistance, and refers to an impaired response to insulin primarily in muscle, liver, and fat. Both situations cause glucose to accumulate in the blood, which in the long run can damage organs, including the brain. Specifically, high blood glucose levels can damage brain blood vessels and nerves, leading to problems with memory, learning, and mood[9-11].
Multiple epidemiological studies suggest an association between type 2 diabetes and a higher risk of developing Alzheimer’s disease[12-14]. According to a 2021 study in the U.K. that included 10,000 people, developing type 2 diabetes at a younger age increases the risk of future dementia[15]. In addition, a study of brain tissue from deceased Alzheimer’s patients suggest that high levels of insulin and glucose in the blood might accelerate the formation of amyloid plaques in the brain[16].
Diabetes and Alzheimer’s involve some common molecular mechanisms[17], including inflammation and accumulation of amyloid proteins in the affected organ, amylin in the pancreas and beta-amyloid in the brain. Moreover, insulin resistance also occurs frequently in the brains of both diabetic and non-diabetic patients[16,18], and has also been observed in genetic mice models of Alzheimer’s disease that received a high-fat diet[19,20]. Injecting insulin in these animals improved cognitive decline and amyloid accumulation[21].
However, contrary to what the video claimed, the nature of the association between diabetes and Alzheimer’s isn’t well-established. For example, peripheral insulin resistance doesn’t necessarily translate into insulin resistance in the brain. Also, scientists still don’t know whether insulin resistance can cause or accelerate Alzheimer’s disease, or if it is Alzheimer’s that causes dysregulation of glucose metabolism instead[12,13]. For example, a 2000 study published in Science showed that a mouse model for brain insulin resistance developed metabolic problems, including high insulin levels in blood and peripheral insulin resistance[22].
So-called “type 3 diabetes” isn’t a recognized health condition. It is a term that some researchers have proposed to refer specifically to diabetic patients who also develop dementia, based on the still-unconfirmed hypothesis that peripheral insulin resistance can cause Alzheimer’s by leading to insulin resistance in the brain[23].
In the last years, researchers have been investigating drugs that target insulin signaling as a potential treatment for Alzheimer’s. While some clinical trials showed that intranasal administration of insulin improved memory and cognition in healthy adults and Alzheimer’s patients[24,25], the claim that insulin treatment “reversed stages of Alzheimer’s” is an overstatement.
There is currently no evidence demonstrating that insulin treatment can reverse brain damage or improve cognition and survival in Alzheimer’s patients in the long term. In addition, more recent and larger trials showed no benefit from insulin compared to placebo in Alzheimer’s patients over a period of 12 months[26,27]. Therefore, more research is needed to evaluate the therapeutic effect of insulin treatment in Alzheimer’s patients.
Although some medicines can temporarily improve Alzheimer’s symptoms in some people, there is currently no treatment that can prevent, stop, or delay cognitive decline. As of August 2022, there were about 150 drugs in clinical trials for Alzheimer’s disease, including one targeting insulin resistance and glucose metabolism. But even if some of them show to be effective, they will still need time until they can reach patients.
In parallel to the search for drugs that can modify the disease’s onset, progression, and severity, knowledge about risk factors contributing to Alzheimer’s has also increased. Such factors include diabetes, obesity, high blood pressure, sedentarism, smoking, lack of cognitive stimulation, and diet, among others. People can take steps to reduce their risk of developing Alzheimer’s or delay its onset by modifying those risk factors, such as engaging in physical activity and mental exercises.
However, taking steps to reduce one’s risk isn’t the same as preventing the disease entirely, since even some people who otherwise lead healthy lives can still end up developing the disease. Therefore, the claim that “Alzheimer’s most of the time is preventable” is unsupported by available evidence. In fact, a 2020 report by The Lancet Commission on dementia prevention, intervention, and care explained that “Not all dementia will be preventable”. The report suggested that targeting 12 known modifiable factors, including diabetes, obesity, hypertension, tobacco and alcohol consumption, physical activity, and education, among others, could theoretically prevent or delay only 40% of the cases of dementia worldwide.
The claim that insulin resistance causes Alzheimer’s and that restoring insulin sensitivity can prevent most cases of Alzheimer’s is currently unsupported by available evidence. Indeed, brain insulin plays essential roles in memory and learning. Also, type 2 diabetes is a risk factor for developing Alzheimer’s. But a potential role of peripheral and brain insulin resistance in Alzheimer’s is a hypothesis that is under investigation. There is so far no evidence indicating that insulin resistance causes Alzheimer’s; multiple other factors, including genetics and lifestyle factors, also contribute to the likelihood that a person develops the disease.
Alzheimer’s disease
Published on: 15 Oct 2022 | Editor: Iria Carballo-Carbajal
Health Feedback is a non-partisan, non-profit organization dedicated to science education. Our reviews are crowdsourced directly from a community of scientists with relevant expertise. We strive to explain whether and why information is or is not consistent with the science and to help readers know which news to trust.
Please get in touch if you have any comment or think there is an important claim or article that would need to be reviewed.
Get email news updates:
Follow us:
See how we rate claims
We depend on your support to operate. Help us create a more trustworthy Internet!
Donate
Reviewers
Community standards
Apply to become a reviewer
About
Our method to evaluate articles
Our method to evaluate claims
Contact us